Vision News
How community optometry is working with secondary eye care
Working together to care for patients
Scottish optometrist Elaine Hawthorn talks about how working with her hospital ophthalmology colleagues – who are more than a 140-mile round-trip away – is benefiting patients in her community
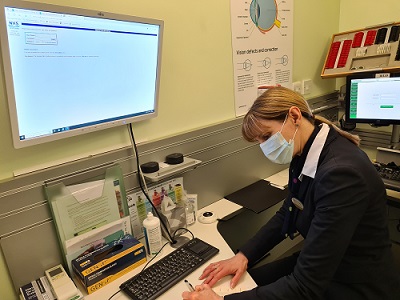
‘I’m based at Specsavers Stranraer, which is the second largest town in Dumfries and Galloway. We cover a pretty rural area. The main hospital eye clinic in Dumfries is more than 70 miles away from us – a more than 140-mile round trip for patients,’ says Elaine.

‘Dumfries and Galloway Royal Infirmary is at one end of the county, and we are at the other. There is a local community hospital in Stranraer, however, there are limited clinics and resources there due to location and ophthalmologist availability, meaning the majority of patients have to travel.’
It’s where Elaine has been able to step in to support patients and the NHS by providing care in the community – something that eye health experts who own local Specsavers practices across the country do as well.
She explains that she has done a lot of Independent Prescribing work since gaining the qualification a decade ago, but that hospital colleagues in the past were not as aware of what optometrists can do, or the knowledge and skills they possess. The pandemic helped change this, she adds, with Specsavers also committed to supporting and upskilling clinicians to deliver incredible patient care.
Community care
‘Over the last few years, through the Covid-19 pandemic, we have built that critical relationship here between community optometry and hospital ophthalmology. They are now aware of just how much we can contribute by working together to improve patient care in the community and thus easing the burden on the hospital eye service, especially in a rural setting.’
Specsavers Stranraer was set up as an emergency treatment centre at the height of the pandemic, she says, and learning from that time has been used to support care of patients in their local community.
Elaine adds: ‘It’s a long way to get to Dumfries. Many eye appointments require drops, so patients are unable to drive but they may be the only driver in their household. They may not have friends or family in a position to take them.
‘With regards to acute issues like uveitis and herpes simplex, often I can treat this without hospital input at all. If the case is more complex, I will usually discuss treatment plans with my hospital colleagues, start treatment and either continue to review myself or the hospital will if they deem it appropriate. This reduces both patient travel and hospital eye service time. This process became more common during Covid due to the importance of keeping patients out of the hospital setting where possible and has continued.’
Elaine – who started her Specsavers career as a student in 1996 – will see patients from time-to-time who are ‘walks-in’ having contacted the hospital eye clinic or local A&E. But most of the time she will get a phone call from the clinic asking if she could look at a patient and then follow-up after treatment.
‘If I can deal with the situation in practice I will, or I can contact the eye clinic by direct line if further assessment or treatment is required.’
The way forward
‘Working together is absolutely the way forward, especially in rural settings where are there are particular challenges around recruitment of ophthalmologists and nurses – where one of them being off ill for example throws hospital clinics off. They don’t have capacity to absorb any more patients,’ says Elaine.
‘It’s great having that relationship because it can be a two-way thing. They quite often phone and ask me for help. So, I’m quite happy to phone and ask them for help.
‘It’s made a huge difference. We are also part of a glaucoma monitoring scheme. Many patients find this much easier than attending the hospital. They are able to come to a local community practice rather than making the two-hour journey to Dumfries for a short review appointment. This is likely to improve attendance and therefore help save sight as well.
‘Funding in Scotland for optometry also helps enable this joined-up working, and it is something that would benefit patients in the rest of the UK as well.’